Assessing Coronary Artery Disease Using FFR
Assessing Coronary Artery Disease Using FFR
CORONARY artery disease implies the presence of narrowing or blockages within the arteries that supply oxygen and nutrients to the heart muscles. At present, a coronary angiogram remains the gold standard for the assessment of coronary artery disease. While it may be an invasive procedure, the overall risk of major complications associated with a coronary angiogram remains very low.
A fractional flow reserve (FFR) is an assessment performed as an extension to a coronary angiogram to determine the significance of a particular blockage. The significance of a blockage would depend on the location of the blockage within an artery. If the blockage is at the beginning of the artery, it would lead to more problems as opposed to it being at the end of the artery.
Think of the artery as a water hose with numerous connections to other water sprinklers in the middle of the hose. If there is a blockage at the beginning of the hose, then the effect would be more detrimental as compared to the presence of a blockage at the end of the hose.
Blockages of a similar degree may also confer different consequences if they are present in different arteries as some arteries are larger and are more important compared to the rest.
The FFR assessment is performed using a wire known as a pressure wire. On the wire, there is a pressure sensor located close to its tip to measure the pressure within the artery itself. Pressure will first be measured at the beginning of the artery and once this is done, the pressure wire will then be passed across the blockage to remeasure the pressure after the administration of a medication to ensure that blood flow through the artery is maximal. The FFR is a ratio whereby the pressure after the blockage is divided by the pressure at the beginning of the artery.
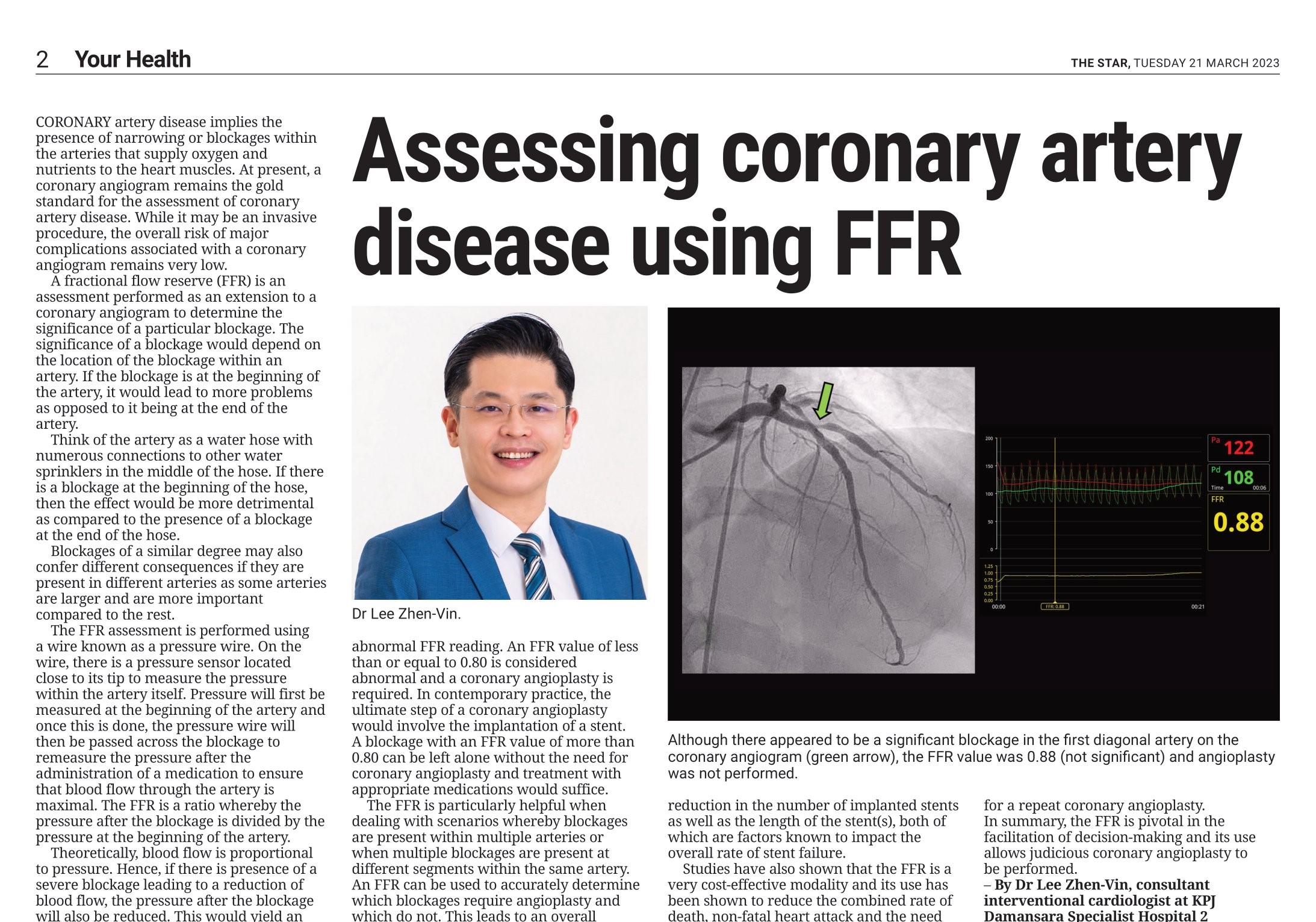
Theoretically, blood flow is proportional to pressure. Hence, if there is presence of a severe blockage leading to a reduction of blood flow, the pressure after the blockage will also be reduced. This would yield an abnormal FFR reading. An FFR value of less than or equal to 0.80 is considered abnormal and a coronary angioplasty is required. In contemporary practice, the ultimate step of a coronary angioplasty would involve the implantation of a stent. A blockage with an FFR value of more than 0.80 can be left alone without the need for coronary angioplasty and treatment with appropriate medications would suffice.
The FFR is particularly helpful when dealing with scenarios whereby blockages are present within multiple arteries or when multiple blockages are present at different segments within the same artery. An FFR can be used to accurately determine which blockages require angioplasty and which do not. This leads to an overall reduction in the number of implanted stents as well as the length of the stent(s), both of which are factors known to impact the overall rate of stent failure.
Studies have also shown that the FFR is a very cost-effective modality and its use has been shown to reduce the combined rate of death, non-fatal heart attack and the need for a repeat coronary angioplasty.
In summary, the FFR is pivotal in the facilitation of decision-making and its use allows judicious coronary angioplasty to be performed.
– By Dr Lee Zhen-Vin, Consultant
Interventional Cardiologist at Damansara Specialist Hospital 2
For more information, contact 03-7717 3000.




 Promotion
Promotion
 Find Doctor
Find Doctor


